A new paper entitled "Quantitative CT Characteristics of Cluster Phenotypes in the Severe Asthma Research Program Cohorts" was just published in the Radiology. This paper shows the utility of biomechanical measures (especially Jacobian and ADI) in clustering and phenotyping asthma subgroups.
Background: Clustering key clinical characteristics of participants in the Severe Asthma Research Program (SARP), a large, multi-center prospective observational study of patients with asthma and healthy controls, has led to the identification of novel asthma phenotypes.
Purpose: To determine whether quantitative CT (qCT) could help distinguish between clinical asthma phenotypes.
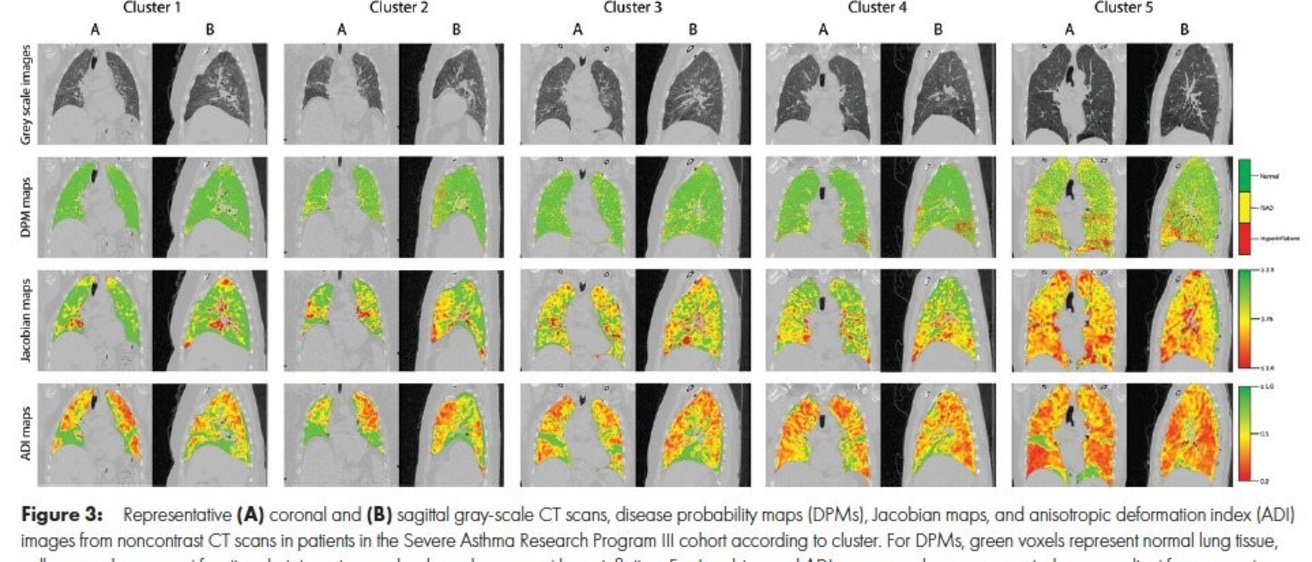
Materials and Methods: A retrospective cross-sectional analysis was conducted with the use of qCT images (maximal bronchodilation at total lung capacity [TLC], or inspiration, and functional residual capacity [FRC], or expiration) from the cluster phenotypes of SARP participants (cluster 1: minimal disease; cluster 2: mild, reversible; cluster 3: obese asthma; cluster 4: severe, reversible; cluster 5: severe, irreversible) enrolled between September 2001 and December 2015. Airway morphometry was performed along standard paths (RB1, RB4, RB10, LB1, and LB10). Corresponding voxels from TLC and FRC images were mapped with use of deformable image registration to characterize disease probability maps (DPMs) of functional small airway disease (fSAD), voxel-level volume changes (Jacobian), and isotropy (anisotropic deformation index [ADI]). The association between cluster assignment and qCT mea-sures was evaluated using linear mixed models.
Results: A total of 455 participants were evaluated with cluster assignments and CT (mean age 6 SD, 42.1 years 6 14.7; 270 women). Airway morphometry had limited ability to help discern between clusters. DPM fSAD was highest in cluster 5 (cluster 1 in SARP III: 19.0% 6 20.6; cluster 2: 18.9% 6 13.3; cluster 3: 24.9% 6 13.1; cluster 4: 24.1% 6 8.4; cluster 5: 38.8% 6 14.4; P, .001). Lower whole-lung Jacobian and ADI values were associated with greater cluster severity. Compared to cluster 1, cluster 5 lung expansion was 31% smaller (Jacobian in SARP III cohort: 2.31 6 0.6 vs 1.61 6 0.3, respectively, P, .001) and 34% more isotropic (ADI in SARP III cohort: 0.40 6 0.1 vs 0.61 6 0.2, P, .001). Within-lung Jacobian and ADI SDs decreased as severity worsened (Jacobian SD in SARP III cohort: 0.90 6 0.4 for cluster 1; 0.79 6 0.3 for cluster 2; 0.62 6 0.2 for cluster 3; 0.63 6 0.2 for cluster 4; and 0.41 6 0.2 for cluster 5; P, .001).
Conclusion: Quantitative CT assessments of the degree and intraindividual regional variability of lung expansion distinguished between well-established clinical phenotypes among participants with asthma from the Severe Asthma Research Program study.